Trend of adjusted antenatal care visits on pregnant women and neonatal during the COVID-19 pandemic
Findings from a three districts survey in 2021
DOI:
https://doi.org/10.24252/al-sihah.v17i2.58893Keywords:
antenatal care, covid-19, interrupted time series, maternal health, neonatal birthAbstract
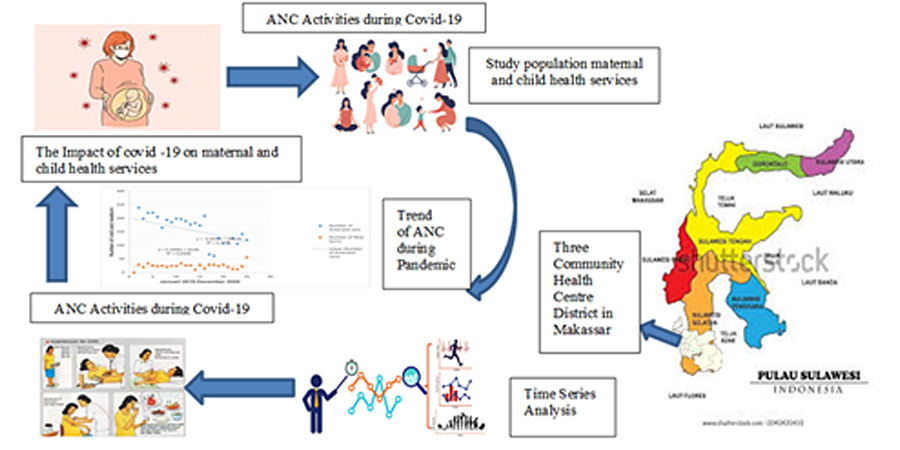
Sustainable health development efforts amid infectious disease outbreaks such as Coronavirus disease 2019 (COVID-19) require a resilient maternal health system. With cases rising globally and across Asia, Indonesia faces significant disruptions in essential services. A critical research gap exist in utilizing adjusted time-series analysis to isolated pandemic impact from seasonal variation in urban Indonesia. This study evaluates trends in antenatal care (ANC) visits (January 2019–December 2020) at three Community Health Centres in Makassar: Bara-Baraya, Jongaya and Batua using Interrupted Time Series (ITS) analysis. Findings reveal a significant decline in visits during the second and third quarters of 2020, primarily due to transmission fears. We suggest integration of telemedicine and home visits to maintain continuity of care. Although focused on urban Makassar, these results are an important reference for health and offer applicable solutions for other developing countries facing resource constraints. This study emphasizes the need for inclusive prevention strategies to protect maternal health in urban and rural areas in low- to middle-income countries during systemic health crises.
Downloads
References
Ariani N. Antenatal care services utilization during COVID-19 second wave attack in Pasuruan, Indonesia. (2022). J Med Life,15(1):7–14. https://doi.org/10.25122/jml-2021-0238.
Fridell M, Edwin S, von SJ, Saulnier DD. (2020). Health system resilience: what are we talking about? A scoping review mapping characteristics and keywords. Int J Health Policy Manag, 1;9(1):6–16. https://doi.org/10.1093/ije/dyw098.
Central Bureau Statistic. South Sulawesi Province in Figures. (2019). https://sulsel.bps.go.id/publication/2019/08/16/990caae13d6f4c5d743e852b/provinsi-sulawesi-selatan-dalam-angka-2019.html.
Chu, Dinh Toi, Suong Mai Vu Ngoc, Hue Vu Thi, Yen Vy Nguyen Thi, Thuy Tien Ho, Van Thuan Hoang, Vijai Singh, and Jaffar A. Al-Tawfiq. (2022). “COVID-19 in Southeast Asia: Current Status and Perspectives.” Bioengineered 13(2):3797–3809.
Downey LE, Gadsden T, Del V, Vilas R, Peiris D, Jan S. (2022). The impact of COVID-19 on essential health service provision for endemic infectious diseases in the South-East Asia region: A systematic review. The Lancet Regional Health-Southeast Asia,1:100011. https://doi.org/10.1016/j.
Drummond, Nora, Joanne Bailey, Christina Majszak, and Ruth Zielinski. (2024). “Implementation of Virtual Antenatal and Postnatal Urgent Midwifery Visits: Evaluation of a Quality Improvement Initiative.” International Journal of Environmental Research and Public Health 21(7). https://www.doi.org/10.3390/ijerph21070903
Eurosurveillance Editorial Team. (2020). “Note from the Editors: World Health Organization Declares Novel Coronavirus (2019-NCoV) Sixth Public Health Emergency of International Concern.” Euro Surveillance : Bulletin Europeen Sur Les Maladies Transmissibles = European Communicable Disease Bulletin 25(5). https://www.doi.org/10.2807/1560-7917.ES.2020.25.5.200131e
Fridell M, Edwin S, von SJ, Saulnier DD. (2020). Health system resilience: what are we talking about? A scoping review mapping characteristics and keywords. Int J Health Policy Manag, 1;9(1):6–16. https://doi.org/10.15171/ijhpm.2019.71
Golden, Bethany N., Shaimaa Elrefaay, Monica R. McLemore, Amy Alspaugh, Kimberly Baltzell, and Linda S. Franck. (2024). “Midwives’ Experience of Telehealth and Remote Care: A Systematic Mixed Methods Review.” BMJ Open 14(3). https://www.doi.org/10.1136/bmjopen-2023-082060
Goyal M, Singh P, Singh K, Shekhar S, Agrawal N, Misra S. (2021). The effect of the COVID-19 pandemic on maternal health due to delay in seeking health care: Experience from a tertiary center. International Journal of Gynecology and Obstetrics, 152(2):231–5. https://doi.org/10.1002/ijgo.13457
Haldane V, Foo C, Abdalla SM, Jung AS, Tan M, Wu S. (2021). Health systems resilience in managing the COVID-19 pandemic: lessons from 28 countries. Nature Medicine Nature Research, 27:964–80. https://doi.org/10.1038/s41591-021-01381-y.
Indonesia Ministry Health. (2020). Protocol of Healthy Mothers and New Baby Born Services During Pandemic COVID-19. https://infeksiemerging.kemkes.go.id/download/
Kikuchi K, Yi S, Nanishi K, Yasuoka J. (2024). Challenges of Maternal and Child Health after the COVID-19 Pandemic. Frontiers Media SA, 2024. (Frontiers Research Topics). https://doi.org/10.3389/978-2-8325-4385-6.
Kotlar, Bethany, Emily Gerson, Sophia Petrillo, Ana Langer, and Henning Tiemeier. (2021). “The Impact of the COVID-19 Pandemic on Maternal and Perinatal Health: A Scoping Review.” Reproductive Health 18(1).
Lang’At E, Mwanri L, Temmerman M. (2019). Effects of implementing free maternity service policy in Kenya: An interrupted time series analysis. BMC Health Serv Res. 19(1). https://doi.org/10.1186/s12913-019-4462-x.
Manjavidze T, Rylander C, Egil Skjeldestad F, Kazakhashvili N, Anda EE. (2020). The impact of antenatal care utilization on admissions to neonatal intensive care units and perinatal mortality in Georgia. PLoS One, 1;15 (12 December). https://doi.org/10.1371/journal.pone.0242991.
Miskeen E. (2024). Utilization of Antenatal Care Services Within the Context of COVID-19, Security Challenges, and an Unstable Healthcare System at Primary Health Care Centers. Int J Womens Health, 16:737–47. https://doi.org/10.2147/IJWH.S435894.
Murewanhema G, Mpabuka E, Moyo E, Tungwarara N, Chitungo I, Mataruka K. (2023) Accessibility and utilization of antenatal care services in sub-Saharan Africa during the COVID-19 pandemic: A rapid review, 50:496–503. https://doi.org/10.1111/birt.12719.
Peahl AF and Howell JD. (2021). The evolution of prenatal care delivery guidelines in the United States. American Journal of Obstetrics and Gynecology Mosby Inc. 224:339–47. https://doi.org/10.1016/j.ajog.2020.12.016
Provincial Health Office. South Sulawesi FY. South Sulawesi Provincial Health Office Performance Report (LKOJ). https://e-renggar.kemkes.go.id/file_performance/1-199003-2tahunan-488.pdf
Safo, Kwame S., Daniel Opoku, Richard A. Bonney, Clement K. Serchim, and Kofi A. Mensah. (2025). “Potential Effects of Whatsapp on Maternal Health Services Uptake during COVID-19: A Cross-Sectional Study in Ghana.” BMC Health Services Research 25(1). https://doi.org/10.1186/s12913-025-12245-3
Singh A, Jain P, Singh N, Kumar S, Bajpai P, Singh S. (2021). Impact of COVID-19 pandemic on maternal and child health services in Uttar Pradesh. India J Family Med Prim Care, 10(1). https://doi.org/10.4103/jfmpc.jfmpc_1550_20
Thompson, Madeline, Amanda K. Buttery, Shu Xin Oh, Macy Chan, Byung Hyun Lee, Tomoharu Iino, Yu Chun Alice Wang, and Chris Clarke. (2025). “Risk Factors for Severe COVID-19 Outcomes in the Asia-Pacific Region: A Literature Review.” Frontiers in Public Health 13
Tounkara M, Sangho O, Beebe M, Whiting-Collins LJ, Goins RR, Marker HC.(2022). Geographic Access and Maternal Health Services Utilization in Sélingué Health District, Mali. Matern Child Health J, 26(3):649–5. https://doi.org/10.1007/s10995-021-03364-4
Thirugnanasundralingam K, Davies-Tuck M, Rolnik DL, Reddy M, Mol BW, Hodges R. (2023). Effect of telehealth-integrated antenatal care on pregnancy outcomes in Australia: an interrupted time-series analysis. Lancet Digit Health, https://doi.org/10.1016/S2589-7500(23)00151-6.
Vermeulen J, Bilsen J, Buyl R, Smedt D, Gucciardo L, Faron G. (2022). Women’s experiences with being pregnant and becoming a new mother during the COVID-19 pandemic. Sexual and Reproductive Healthcare, 1;32. https://doi.org/10.1016/j.srhc.2022.100728
Wilhelm JA and Helleringer S. (2019). Utilization of non-Ebola health care services during Ebola outbreaks: A systematic review and meta-analysis. J Glob Health, 9(1). https://doi.org/10.7189/jogh.09.010406.
World Health Organization. (2020) Health workforce policy and management in the context of the COVID-19 pandemic response Interim guidance. https://iris.who.int/bitstream/handle/10665/337333/WHO-2019-nCoV-health_workforce-2020.1-eng
World Health Organization, and Human Reproduction Programme. 2024. Roadmap for Research on Maternal and Perinatal Health in the Context of Epidemic Threats.
Wu H, Sun W, Huang X, Yu S, Wang H, Bi X. (2020). Online antenatal care during the COVID-19 pandemic: Opportunities and challenges. Journal of Medical Internet Research, 22. https://doi.org/10.2196/19916
Published
How to Cite
Issue
Section
License
Copyright (c) 2025 Juliani Ibrahim, Yoko Takahata, Sukaeni Ibrahim

This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.
Authors retain copyright and grant the journal right of first publication with the work simultaneously licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License that allows others to share the work with an acknowledgment of the work's authorship and initial publication in this journal.
Authors are able to enter into separate, additional contractual arrangements for the non-exclusive distribution of the journal's published version of the work (e.g., post it to an institutional repository or publish it in a book), with an acknowledgment of its initial publication in this journal.
Authors are permitted to publish their work online in third parties as it can lead to wider dissemination of the work.