Family support and quality of life among urban elderly people
A cross-sectional study in Dhaka, Bangladesh
DOI:
https://doi.org/10.24252/al-sihah.v17i2.61825Keywords:
aged, Bangladesh, family support , quality of life , urban populationAbstract
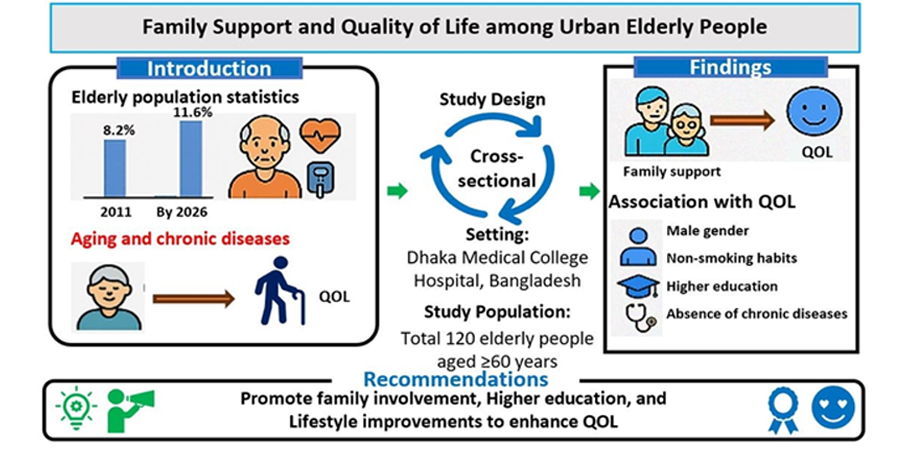
In Bangladesh, the elderly population is expected to rise from 8.2% in 2011 to 11.6% in 2026, which is associated with an increasing burden of chronic diseases that negatively affect the quality of life of the elderly. Previous research on the quality of life (QOL) of the elderly in Bangladesh has given limited focus on the elderly in urban settings within a healthcare setting and the impact of family support. This study aimed to examine the relationship between family support and quality of life among urban elderly people in Bangladesh. A hospital-based cross-sectional study was done among elderly attendants of Dhaka Medical College Hospital with convenience sampling. Data collection was done using a structured questionnaire consisting of socio-demographic data, Family Support Scale (FSS) and WHOQOL-BREF Scale. Statistical analyses, such as independent t-tests, Pearson’s correlation and ANOVA, were performed. About half of the respondents perceived poor family support, and 46.7% had poor overall QOL. Family support was found to have a significant positive correlation with QOL (r = 0.754, p < 0.01). Male gender (p = 0.024), higher education (p < 0.01), absence of chronic disease (p < 0.01), non-smoker (p < 0.01) and joint family living (p < 0.01) were found to be significantly associated with better QOL. These results emphasize the need to strengthen family support and chronic disease management in the city, and suggest that reinforcement of traditional family networks as well as improving access to healthcare may improve the quality of life in the elderly rural populations.
Downloads
References
Bangladesh Bureau of Statistics. (2022). POPULATION & HOUSING CENSUS 2022. https://sid.portal.gov.bd/sites/default/files/files/sid.portal.gov.bd/publications/01ad1ffe_cfef_4811_af97_594b6c64d7c3/PHC_Preliminary_Report_(English)_August_2022.pdf
Bikrant, J., Prusty, K., Kumar, A., Varma, P., & Kedarnath Navandar, R. (2022). Analyzing the Influence of Health-Related Factors on Quality of Life among Elderly Populations. Health Leadership and Quality of Life, ISSN-e 3008-8488, Vol. 1, No. 0, 2022 (Ejemplar Dedicado a: Health Leadership and Quality of Life), 1(0), 59. https://doi.org/10.56294/HL2022146SOFTWARE
Bodiuzzaman, M., Rahman, A., Islam, M. D., Miah, M. N. A., & Chowdhury, R. Sen. (2022). Prevalence of Comorbidities among Elderly Patients in a General Hospital of Bangladesh. Bangladesh Journal of Medicine, 33(3), 269–273. https://doi.org/10.3329/BJM.V33I3.61373
Cadmus, E. O., Adebusoye, L. A., & Owoaje, E. T. (2021). Rural–urban differences in quality of life and associated factors among community-dwelling older persons in Oyo state, South-Western Nigeria. Quality & Quantity, 56(3), 1327–1344. https://doi.org/10.1007/S11135-021-01178-8
De Maria, M., Tagliabue, S., Ausili, D., Vellone, E., & Matarese, M. (2020). Perceived social support and health-related quality of life in older adults who have multiple chronic conditions and their caregivers: a dyadic analysis. Social Science & Medicine (1982), 262. https://doi.org/10.1016/J.SOCSCIMED.2020.113193
Dewi, C. F., Marlina, Y. F., & Dafiq, N. (2025). Family Support and Loneliness in The Elderly: Their Influence on Quality of Life. Dunia Keperawatan: Jurnal Keperawatan Dan Kesehatan, 13(1), 68–74. https://doi.org/10.20527/jdk.v13i1.781
Faul, F., Erdfelder, E., Lang, A. G., & Buchner, A. (2007). G*Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behavior Research Methods 2007 39:2, 39(2), 175–191. https://doi.org/10.3758/BF03193146
Gil-Lacruz, M., Cañete-Lairla, M., Navarro, J., Montaño-Espinoza, R., Espinoza-Santander, I., & Osorio-Parraguez, P. (2022). Validation of the WHOQOL-BREF Quality of Life Questionnaire in an Urban Sample of Older Adults in a Neighbourhood in Zaragoza (Spain). Healthcare 2022, Vol. 10, Page 2272, 10(11), 2272. https://doi.org/10.3390/HEALTHCARE10112272
Grassi, L., Caruso, R., Da Ronch, C., Härter, M., Schulz, H., Volkert, J., Dehoust, M., Sehner, S., Suling, A., Wegscheider, K., Ausín, B., Canuto, A., Muñoz, M., Crawford, M. J., Hershkovitz, Y., Quirk, A., Rotenstein, O., Santos-Olmo, A. B., Shalev, A., … Nanni, M. G. (2020). Quality of life, level of functioning, and its relationship with mental and physical disorders in the elderly: results from the MentDis_ICF65+ study. Health and Quality of Life Outcomes 2020 18:1, 18(1), 61-. https://doi.org/10.1186/S12955-020-01310-6
Hanley, B., Tassé, M. J., Aman, M. G., & Pace, P. (1998). Psychometric properties of the family support scale with head start families. Journal of Child and Family Studies, 7(1), 69–77. https://doi.org/10.1023/A:1022912130180/METRICS
Idris, D. N. T., Taviyanda, D., & Pattipeilohy, K. (2025). Relationship between family support with cognitive function and quality of life in the elderly. Riset Informasi Kesehatan, 14(1), 74. https://doi.org/10.30644/rik.v14i1.950
Islam, M. N., Islam, M. S., Jahan, F., & Akter, K. (2020). Functional Status of Elderly People in Rural Community of Bangladesh. IOSR Journal of Nursing and Health Science (IOSR-JNHS), 9(3), 1–08. https://doi.org/10.9790/1959-0903100108
Jahangir, S., Bailey, A., Hassan, Md. M. U., & Hossain, S. (2025). Population Aging and Everyday Challenges for Older Adults in Bangladesh. Handbook of Aging, Health and Public Policy, 131–146. https://doi.org/10.1007/978-981-99-7842-7_170
Jeong, Y., & Kim, Y.-J. (2023). The Effects of Family Support Activities on Life Satisfaction in the Elderly. Asia-Pacific Journal of Convergent Research Interchange, 9(5), 267–277. https://doi.org/10.47116/apjcri.2023.05.23
Kalfoss, M. H., Reidunsdatter, R. J., Klöckner, C. A., & Nilsen, M. (2021). Validation of the WHOQOL-Bref: psychometric properties and normative data for the Norwegian general population. Health and Quality of Life Outcomes 2021 19:1, 19(1), 13-. https://doi.org/10.1186/S12955-020-01656-X
Karmacharya, I., Ghimire, S., Tuladhar, L., Mistry, S. K., Yadav, O. P., Prasai, S., Mehata, S., & Yadav, U. N. (2025). Family Support Paradox: Exploring Family Support and Life Satisfaction Among Older Adults in Rural Eastern Nepal. Behavioral Sciences, 15(4), 411. https://doi.org/10.3390/BS15040411/S1
Knodel, J., & Teerawichitchainan, B. (2017). Family support for older persons in Thailand: Challenges and opportunities. In Research Collection School of Social Sciences (Issue 3). Population Studies Center, Report No. 17-879. https://ink.library.smu.edu.sg/soss_research/2439
Lima, S., Teixeira, L., Esteves, R., Ribeiro, F., Pereira, F., Teixeira, A., & Magalhães, C. (2020). Spirituality and quality of life in older adults: a path analysis model. BMC Geriatrics, 20(1). https://doi.org/10.1186/S12877-020-01646-0
Liu, H., Gan, Q., Tan, J., Sun, X., Liu, Y., & Wan, C. (2023). The association between quality of life and subjective wellbeing among older adults based on canonical correlation analysis. Frontiers in Public Health, 11. https://doi.org/10.3389/FPUBH.2023.1235276
Mayasari, A. C., Rohmah, L., Syadiyah, H., Kirana, S. A. C., Mutyah, D., & Poddar, S. (2022). Relationship between Family Support and Elderly Independence in Fulfilling Daily Activities. Malaysian Journal of Medical Research (MJMR), 6(4), 15–19. https://doi.org/10.31674/MJMR.2022.V06I04.003
Naing, M. Z., May, S. Y., Aung, M. H., & May, Y. (2020). Caregiver burden from caring for dependent elderly in Yangon, The Republic of the Union of Myanmar. Makara Journal of Health Research, 24(1), 3. https://doi.org/10.7454/msk.v24i1.1067
Nurchayati, S., Utomo, W., & Karim, D. (2019). Correlation between family support and quality of life among hypertensive patients. Enfermería Clínica, 29, 60–62. https://doi.org/10.1016/J.ENFCLI.2018.11.020
Parvin Lasker, S., Tribenee Mithila, T., Hossain, A., Ruhul Amin, M., & Lasker Professor, S. (2023). Senior Citizen’s Understanding regarding the quality of life and policy of Bangladesh. In Journal of Mathematics Instruction, Social Research and Opinion (Vol. 2, Issue 2, pp. 115–128). https://doi.org/10.58421/misro.v2i2.78
Rizal, H., Said, M. A., Majid, H. A., Su, T. T., Pin, T. M., Ismail, R., & Zaidi, M. A. S. (2022). Health-related quality of life of younger and older lower-income households in Malaysia. PLoS ONE, 17(2), e0263751. https://doi.org/10.1371/JOURNAL.PONE.0263751
Shah, V. R., Christian, D. S., Prajapati, A. C., Patel, M. M., & Sonaliya, K. N. (2017). Quality of life among elderly population residing in urban field practice area of a tertiary care institute of Ahmedabad city, Gujarat. Journal of Family Medicine and Primary Care, 6(1), 101. https://doi.org/10.4103/2249-4863.214965
Shawver, Z., Griffith, J. D., Adams, L. T., Evans, J. V., Benchoff, B., & Sargent, R. (2016). An examination of the WHOQOL-BREF using four popular data collection methods. Computers in Human Behavior, 55, 446–454. https://doi.org/10.1016/J.CHB.2015.09.030
Silva, P. A. B., Soares, S. M., Santos, J. F. G., & Silva, L. B. (2014). Cut-off point for WHOQOL-bref as a measure of quality of life of older adults. Revista de Saúde Pública, 48(3), 390. https://doi.org/10.1590/S0034-8910.2014048004912
Singh, A., Palaniyandi, S., Palaniyandi, A., & Gupta, V. (2022). Health related quality of life among rural elderly using WHOQOL-BREF in the most backward district of India. Journal of Family Medicine and Primary Care, 11(3), 1162–1168. https://doi.org/10.4103/JFMPC.JFMPC_1073_21
Snell, D. L., Siegert, R. J., Surgenor, L. J., Dunn, J. A., & Hooper, G. J. (2016). Evaluating quality of life outcomes following joint replacement: psychometric evaluation of a short form of the WHOQOL-Bref. Qual Life Res, 25(1), 51–61. https://doi.org/10.1007/s11136-015-1044-1
Tareque, M. I. (2022). Trends in health expectancy at age 60 in Bangladesh from 1996 to 2016. PLOS ONE, 17(11), e0278101. https://doi.org/10.1371/JOURNAL.PONE.0278101
Teoli, D., & Bhardwaj, A. (2023). Quality Of Life. PubMed, Quality Of Life. https://www.ncbi.nlm.nih.gov/books/NBK536962/
The WHOQOL Group. (1994). The Development of the World Health Organization Quality of Life Assessment Instrument (the WHOQOL). Quality of Life Assessment: International Perspectives, 41–57. https://doi.org/10.1007/978-3-642-79123-9_4
Tsutsumi, A., Izutsu, T., Kato, S., Islam, M. A., Yamada, H. S., Kato, H., & Wakai, S. (2006). Reliability and validity of the Bangla version of WHOQOL-BREF in an adult population in Dhaka, Bangladesh. Psychiatry and Clinical Neurosciences, 60(4), 493–498. https://doi.org/10.1111/J.1440-1819.2006.01537.X
Uddin, A., Jalal, M. B., & Anowarul. (2019). Development of the family support scale (FSS) for elderly people. MOJ Gerontology & Geriatrics, 4(1), 17–20. https://doi.org/10.15406/MOJGG.2019.04.00170
Uddin, M. N., & Islam, F. M. A. (2019). Psychometric evaluation of an interview-administered version of the WHOQOL-BREF questionnaire for use in a cross-sectional study of a rural district in Bangladesh: an application of Rasch analysis. BMC Health Services Research 2019 19:1, 19(1), 216-. https://doi.org/10.1186/S12913-019-4026-0
United Nations, D. of E. and S. A. (2020). International Migrant Stock 2020 Documentation. United Nations Database, POP/DB/MIG/Stock/Rev.2020. www.unpopulation.org.
Urie Bronfenbrenner. (1979). The Ecology of Human Development. The Ecology of Human Development, 7. https://www.hup.harvard.edu/books/9780674224575
Wang, L., Yang, L., Di, X., & Dai, X. (2020). Family Support, Multidimensional Health, and Living Satisfaction among the Elderly: A Case from Shaanxi Province, China. International Journal of Environmental Research and Public Health, 17(22), 8434. https://doi.org/10.3390/IJERPH17228434
Wardani, E. D. A., Retnaningsih, D., & Wulandari, P. (2022). Family Support Related to Quality of Living Elderly with Demensia. Jurnal Ners Widya Husada, 10(2), 403. https://doi.org/10.26714/jkj.10.2.2022.403-410
Wei, A., Bell, J., Locke, J., Roach, A., Rogers, A., Plys, E., Zaguri-Greener, D., Zisberg, A., & Lopez, R. P. (2024). Family Involvement in the Care of Nursing Home Residents With Dementia: A Scoping Review. Journal of Applied Gerontology, 43(11), 1772–1784. https://doi.org/10.1177/07334648241255534
WHO. (2012). WHOQOL - Measuring Quality of Life. World Health Organization. https://www.who.int/tools/whoqol
WHO. (2025). Ageing and health. World Health Organization. https://www.who.int/news-room/fact-sheets/detail/ageing-and-health
Zhang, J., Qing, W., Zhou, Y., Zhou, J., & Xu, F. (2025). The impact of frailty on quality of life among older adults in nursing homes: the mediating role of psychological resilience. Frontiers in Public Health, 13, 1692042. https://doi.org/10.3389/FPUBH.2025.1692042
Zin, P. E., Saw, Y. M., Saw, T. N., Cho, S. M., Hlaing, S. S., Noe, M. T. N., Kariya, T., Yamamoto, E., Lwin, K. T., Win, H. H., & Hamajima, N. (2020). Assessment of quality of life among elderly in urban and peri-urban areas, Yangon Region, Myanmar. PLOS One, 15(10). https://doi.org/10.1371/JOURNAL.PONE.0241211
Published
How to Cite
Issue
Section
License
Copyright (c) 2025 Rakibul Hasan, Deepayan Mondal, Fardina Rahman Omi, Sohel Miah, Bristy Samadder

This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.
Authors retain copyright and grant the journal right of first publication with the work simultaneously licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License that allows others to share the work with an acknowledgment of the work's authorship and initial publication in this journal.
Authors are able to enter into separate, additional contractual arrangements for the non-exclusive distribution of the journal's published version of the work (e.g., post it to an institutional repository or publish it in a book), with an acknowledgment of its initial publication in this journal.
Authors are permitted to publish their work online in third parties as it can lead to wider dissemination of the work.